How Do Ace Inhibitors Work? Benefits Inside
Ace inhibitors, also known as angiotensin-converting enzyme inhibitors, are a class of medications that play a crucial role in managing various cardiovascular conditions, including high blood pressure, heart failure, and coronary artery disease. These medications work by inhibiting the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor that increases blood pressure. In this article, we will delve into the mechanism of action of ace inhibitors, their benefits, and their applications in clinical practice.
Mechanism of Action
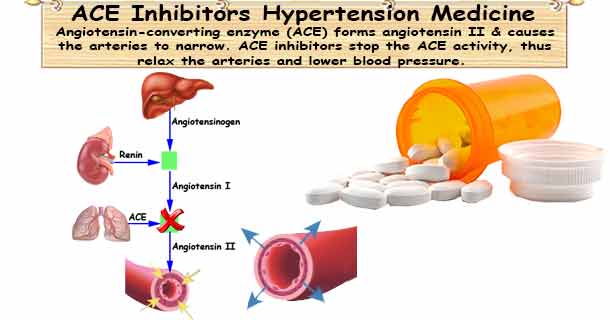
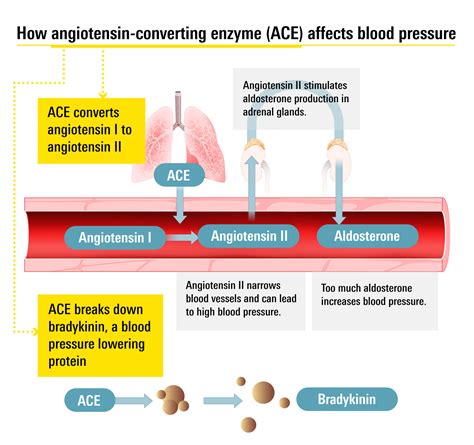
Ace inhibitors exert their effects by blocking the action of angiotensin-converting enzyme (ACE), a naturally occurring enzyme in the body that converts angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor that increases blood pressure by constricting blood vessels and stimulating the release of aldosterone, a hormone that promotes sodium retention and water absorption in the kidneys. By inhibiting the conversion of angiotensin I to angiotensin II, ace inhibitors reduce the levels of angiotensin II, leading to vasodilation and a decrease in blood pressure.
The renin-angiotensin-aldosterone system (RAAS) is a complex physiological pathway that regulates blood pressure, electrolyte balance, and fluid status. Ace inhibitors disrupt this pathway by reducing the levels of angiotensin II, which in turn decreases the release of aldosterone and reduces sodium retention. This leads to an increase in sodium excretion and a decrease in blood volume, further contributing to the reduction in blood pressure.
Pharmacokinetics and Pharmacodynamics
Ace inhibitors are prodrugs, meaning they are converted to their active form in the body. They are absorbed orally and undergo hepatic metabolism to form their active metabolites. The half-life of ace inhibitors varies from 2 to 24 hours, depending on the specific medication. The onset of action is typically within 1-2 hours, with peak effects achieved within 4-6 hours.
The dosage of ace inhibitors varies depending on the specific medication, the indication, and the patient’s renal function. The usual starting dose is 2.5-5 mg daily, with gradual titration to achieve the desired therapeutic effect. The maximum recommended dose varies from 20 to 40 mg daily, depending on the medication.
| Medication | Half-life (hours) | Onset of Action (hours) | Maximum Recommended Dose (mg/day) |
|---|---|---|---|
| Enalapril | 11 | 1-2 | 40 |
| Lisinopril | 12 | 1-2 | 40 |
| Captopril | 2 | 1-2 | 150 |

Clinical Applications

Ace inhibitors are indicated for the treatment of various cardiovascular conditions, including hypertension, heart failure, and coronary artery disease. They are also used to slow the progression of chronic kidney disease and to reduce the risk of stroke and myocardial infarction.
In patients with diabetes, ace inhibitors have been shown to reduce the risk of nephropathy and retinopathy. They are also effective in reducing the risk of cardiovascular events in patients with left ventricular dysfunction and heart failure.
Benefits and Risks
The benefits of ace inhibitors include their ability to reduce blood pressure, decrease cardiovascular morbidity and mortality, and slow the progression of kidney disease. However, they can also cause adverse effects, such as cough, hyperkalemia, and renal dysfunction.
Patients with renal impairment or hyperkalemia should be monitored closely when initiating ace inhibitor therapy. Women of childbearing age should also be cautioned about the potential risks of ace inhibitors during pregnancy.
What are the common side effects of ace inhibitors?
+The common side effects of ace inhibitors include cough, dizziness, headache, and fatigue. Less common side effects include hyperkalemia, renal dysfunction, and angioedema.
Can ace inhibitors be used in patients with kidney disease?
+Ace inhibitors can be used in patients with kidney disease, but they should be monitored closely for signs of renal dysfunction. The dosage may need to be adjusted in patients with severe renal impairment.
Can ace inhibitors be used during pregnancy?
+Ace inhibitors are contraindicated during pregnancy due to the risk of fetal harm. Women of childbearing age should be cautioned about the potential risks of ace inhibitors during pregnancy and should use effective contraception.
In conclusion, ace inhibitors are a class of medications that play a crucial role in managing various cardiovascular conditions. They work by inhibiting the conversion of angiotensin I to angiotensin II, leading to vasodilation and a decrease in blood pressure. While they can cause adverse effects, the benefits of ace inhibitors in reducing cardiovascular morbidity and mortality, slowing the progression of kidney disease, and reducing the risk of stroke and myocardial infarction make them a valuable addition to the treatment of various cardiovascular conditions.
