Preemie Bili Recs: Reduce Jaundice Risks
Preterm infants, or preemies, are at a higher risk for jaundice due to their immature liver and increased red blood cell breakdown. Jaundice, characterized by high levels of bilirubin in the blood, can lead to serious complications if left untreated, including kernicterus, a form of brain damage. The American Academy of Pediatrics (AAP) has established guidelines for the management of hyperbilirubinemia in preterm infants, which include phototherapy and, in severe cases, exchange transfusion. Early detection and treatment are crucial in reducing the risks associated with jaundice in preemies.
Understanding Jaundice in Preterm Infants

Jaundice is a common condition in newborns, affecting approximately 60% of term infants and 80% of preterm infants. The condition is caused by the breakdown of red blood cells, which releases bilirubin into the bloodstream. In preterm infants, the liver is not mature enough to process bilirubin efficiently, leading to a buildup of the toxin. Bilirubin levels are typically measured using transcutaneous bilirubinometry or blood tests. The AAP recommends that all preterm infants be screened for jaundice at 24-48 hours of life, with subsequent screenings as necessary.
Risk Factors for Jaundice in Preterm Infants
Certain risk factors increase the likelihood of jaundice in preterm infants, including premature birth (less than 37 weeks gestation), low birth weight (less than 2,500 grams), hemolysis (breakdown of red blood cells), and infection. Additionally, preterm infants who receive blood transfusions are at increased risk for jaundice. Understanding these risk factors is essential in identifying preterm infants who require closer monitoring and early intervention.
| Jaundice Risk Factors | Description |
|---|---|
| Premature birth | Less than 37 weeks gestation |
| Low birth weight | Less than 2,500 grams |
| Hemolysis | Breakdown of red blood cells |
| Infection | Bacterial or viral infections |
| Blood transfusions | Receipt of blood transfusions |

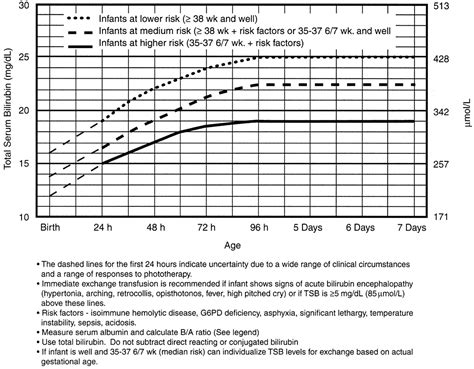
Management of Hyperbilirubinemia in Preterm Infants

The management of hyperbilirubinemia in preterm infants involves a combination of phototherapy, exchange transfusion, and supportive care. Phototherapy, which uses light to break down bilirubin, is the primary treatment for hyperbilirubinemia in preterm infants. Exchange transfusion, which involves replacing the infant’s blood with donor blood, is typically reserved for severe cases of jaundice. Supportive care, including hydration and nutrition, is essential in ensuring the overall health and well-being of the infant.
Phototherapy for Hyperbilirubinemia
Phototherapy is a non-invasive treatment that uses light to break down bilirubin in the skin. The treatment is typically initiated when bilirubin levels reach 15-20 mg/dL, although this may vary depending on the infant’s gestational age and overall health. Intensive phototherapy, which uses high-intensity lights, is often necessary in preterm infants with severe jaundice. The AAP recommends that phototherapy be continued until bilirubin levels decrease to less than 10 mg/dL.
- Initiation of phototherapy: 15-20 mg/dL bilirubin level
- Intensive phototherapy: high-intensity lights for severe jaundice
- Duration of phototherapy: until bilirubin levels decrease to less than 10 mg/dL
What are the risks associated with jaundice in preterm infants?
+The risks associated with jaundice in preterm infants include kernicterus, a form of brain damage, and hearing loss. Untreated jaundice can also lead to seizures, developmental delays, and even death.
How is jaundice diagnosed in preterm infants?
+Jaundice is diagnosed in preterm infants using transcutaneous bilirubinometry or blood tests. The AAP recommends that all preterm infants be screened for jaundice at 24-48 hours of life, with subsequent screenings as necessary.
In conclusion, the management of hyperbilirubinemia in preterm infants requires a comprehensive approach that includes early detection, phototherapy, and supportive care. By understanding the risk factors associated with jaundice and initiating treatment promptly, healthcare providers can reduce the risks associated with this condition and improve outcomes for preterm infants.

